Causes of dyspnoea
Dyspnoea can have a variety of causes, and this means that clinical signs will vary. The Royal Veterinary College reports that the most common causes presenting to their emergency department are pneumonia, congestive heart failure (CHF), asthma, pyothorax and laryngeal paralysis (RVC, 2025). Table 1 highlights other common causes of dyspnoea.
| Disease/anatomical location | Example |
| Upper airway obstruction | Brachycephalic airway syndrome Laryngeal paralysis Foreign body Collapsing trachea Neoplasia Nasopharyngeal polyps |
| Lower airway obstruction | Chronic bronchitis Feline asthma Bronchiectasis Bacteria or virus (Bordetella bronchiseptica, Mycoplasma) |
| Pulmonary parenchymal disease | Pneumonia (bacterial, viral, fungal, parasitic, aspiration) Pulmonary oedema Acute lung injury Pulmonary embolism Interstitial lung disease Pulmonary contusions Neoplasia Inflammatory and immune lung diseases Atelectasis |
| Pleural space disease | Pleural effusion (congestive heart failure, hypoproteinaemia, haemorrhage, neoplasia, pyothorax) Pneumothorax Diaphragmatic hernia Neoplasia |
Clinical signs of dyspnoea
It is important to note that subtle changes may not result in obvious signs
It is important to note that subtle changes may not result in obvious signs. For example, cats diagnosed with significant heart disease may exhibit reduced activity, which can be difficult to assess, either because of concurrent disease or due to their generally sedentary lifestyle. History and signalment can be helpful for diagnosis, as can the presentation of the patient by observing breathing pattern and effort (Table 2).
As already stated, clinical signs vary depending upon the disease process, but may include:
- Tachypnoea, dyspnoea or orthopnoea
- Open-mouth breathing in cats (Figure 1)
- Inability to settle, showing distress
- Collapse
- Cyanosis
- Wheezing
- Sneezing
- Coughing
- Nasal discharge/epistaxis
- Stertor or stridor
| Term | Definition |
| Dyspnoea | Laboured breathing or difficulty breathing |
| Tachypnoea | Increased respiratory rate. Not always associated with hyperventilation and should not be confused with panting |
| Panting | Method to dispel heat. Does not necessarily mean distress in dogs, but it can in cats |
| Orthopnoea | Dyspnoea associated with abnormal posture, ie extended neck, flaring nares and abducted elbows |
| Paradoxical breathing pattern | Exaggerated breathing pattern that involves the thorax and abdomen moving at opposite times |
| Restrictive breathing pattern | Rapid shallow breathing often accompanied by considerable abdominal effort |
| Stertor | Low-pitched, vibrating sound similar to snoring. Can occur on inspiration or expiration |
| Stridor | High-pitched sound caused by narrowed or obstructed airway. Usually occurs on inspiration |
Management and treatment of dyspnoea
The immediate priority is to stabilise the patient presenting in respiratory distress. This can be achieved by increasing oxygenation and minimising stress. Sedation may be necessary for anxious patients. The following guide may be helpful.
From initial client contact (telephone)
- Prepare oxygen supply: ideally, this should be in a quiet place, but somewhere that allows easy observation. The method of oxygen delivery should not stress the patient
- Prepare equipment for intravenous catheterisation and intubation
On arrival at the clinic
- The patient should be carried from the door/car to the oxygen supply
Initial stabilisation
Vascular access is highly desirable but should only be attempted if the patient can tolerate it
- Establish a patent airway: emergency intubation or tracheostomy may be necessary
- Provide oxygen in the most efficient manner possible: examples include oxygen kennels or incubators which provide a great oxygen-rich environment, and may be best practice for patients that cannot be handled. However, if they are not specially designed units, heat and moisture will need to be assessed regularly, while minimising the number of times the oxygen seal is broken. Nasal prongs are great for larger breed dogs, if they tolerate them. Alternatively, flow by oxygen with or without a mask can increase inspired oxygen if no specific oxygen kennel is available
- Minimise stress
- Vascular access is highly desirable but should only be attempted if the patient can tolerate it. For example, it may be preferable to sedate a patient in CHF before attempting to gain venous access. However, for patients that need immediate intubation, venous access must be achieved without delay.
Evaluating oxygenation levels and ventilation efficacy
While physical examination and assessment of respiratory rate and effort are invaluable, especially to identify trends and guide treatment, they are unable to give information on ventilation capability. An important step in managing the dyspnoeic patient is understanding the degree of respiratory compromise, which will guide handling, indicate if supplemental oxygen is helpful and guide the safest or best technique if sedation or anaesthesia is needed.
The most effective way to evaluate ventilation is by arterial blood gas analysis, which measures PaO2, carbon dioxide (PaCO2) and acid-base balance
Pulse oximetry is a non-invasive way to assess oxygen saturation levels (SpO2). However, arterial partial pressure (PaO2) may have fallen considerably before a change in SpO2 is seen. The most effective way to evaluate ventilation is by arterial blood gas analysis, which measures PaO2, carbon dioxide (PaCO2) and acid-base balance. This method is not available in all veterinary settings, meaning that the nurse is reliant upon physical observation and recording trends.
Physical examination
Examination will be needed to allow for diagnosis and enable a treatment plan. While this occurs it is crucial to minimise stress, as stress increases oxygen demand just at the time when the body is unable to respond. Understandably, the clinician’s focus will be on diagnosis, which means that the nurse should be managing the environment and watching the patient for signs of deterioration. Sedation may be necessary, and the patient allowed to rest. Low-dose butorphanol is recommended (0.1 to 0.2mg/kg intramuscularly) (Cole, 2018).
Diagnostic tests
Another crucial aspect of managing the dyspnoeic patient is the procurement of diagnostic tests; again, the role of the nurse is to ensure that these are done as safely as possible. Discussion with the clinician should occur before the patient is handled, so that equipment can be prepared and a plan agreed.
Dependent on presentation and diagnosis, diagnostic tests will vary. For example, routine haematology and biochemistry may highlight inflammatory or infectious disease; oropharyngeal polymerase chain reaction (PCR) tests may be useful for parasites, viruses and mycoplasmal disease; or faecal testing might be suggested for Angiostrongylus vasorum in coughing dogs.
Planning for diagnostic tests
For most patients with respiratory disease, some form of imaging will be required. Radiography and ultrasound are most commonly used in general practice, but computed tomography (CT) is widely available at referral centres. CT is more expensive for the client but has the benefit of superior image quality. If the patient needs to be transferred to a referral or 24-hour hospital, consideration should be given to the patient’s ability to travel.
Before diagnostic tests take place, discussion and planning with the clinician should include:
- Type of imaging to be used
- Confirmation of areas of interest and exact images required. This is essential as lung function can be compromised if placed in lateral recumbency before sternal images are taken
- Identification and preparation of necessary equipment
- Keeping the procedure as short as possible, while ensuring that all tests are performed. This should include discussion about tests that may be needed in the future, so that the number of sedations/anaesthetics is limited
- Whether sedation or anaesthesia is necessary or preferred. A drug protocol should be agreed upon, with consideration given to the depressive effect of some drug combinations on respiration
- If chemical restraint is not used, then consideration should be given to increased levels of stress and a possibility of poorer image quality (movement blur, rotation and less likelihood of inspiratory images), which might compromise interpretation
- Protocol for recovery, especially considering some patients will have improved their oxygenating capacity while anaesthetised
- Steps to be taken if the patient deteriorates
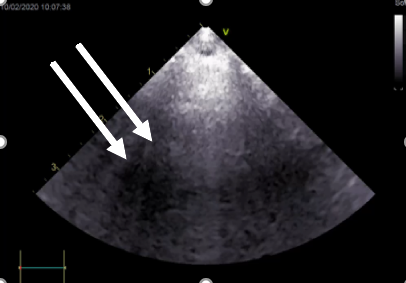
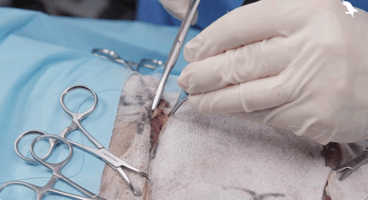
Lung ultrasound is more widely used in general practice and has the advantage of being carried out on the conscious patient. In the healthy patient, very little should be seen on ultrasound, but if there is fluid in the alveoli, B-lines may be seen (Figure 2). Ultrasound also allows for the identification of masses, and highlights if pleural effusion is present. It can then also be used to guide sampling or therapeutic thoracocentesis. Other types of imaging may be required, and sampling performed. Examples include thoracoscopy, rhinoscopy, bronchoscopy and bronchoalveolar lavage.
In the healthy patient, very little should be seen on ultrasound, but if there is fluid in the alveoli, B-lines may be seen
Final thoughts
The veterinary nurse has a crucial role in the management and treatment of the dyspnoeic patient, ranging from telephone triage to initial stabilisation, performing or assisting with diagnostic tests and/or monitoring anaesthesia. As with any emergency, collaboration with colleagues is imperative to allow for the best possible outcome.
References (click to expand)
| Cole, L. | 2018 | Emergency management of dyspnoea. Veterinary Ireland Journal, 11, 600-606 |
| Good, J. M. and King, L. G. | 2010 | Clinical approach to respiratory distress. In: Luis Fuentes, V., Johnson, L. R. and Dennis, S. (eds), BSAVA Manual of Canine and Feline Cardiorespiratory Medicine, 2nd ed. British Small Animal Veterinary Association, Gloucester |
| RVC | 2025 | Respiratory distress in cats and dogs. Royal Veterinary College [Accessed: May 2025] |
| Sharp, C. R. | 2015 | Approach to respiratory distress in dogs and cats. Today’s Veterinary Practice. [Accessed: May 2025] |